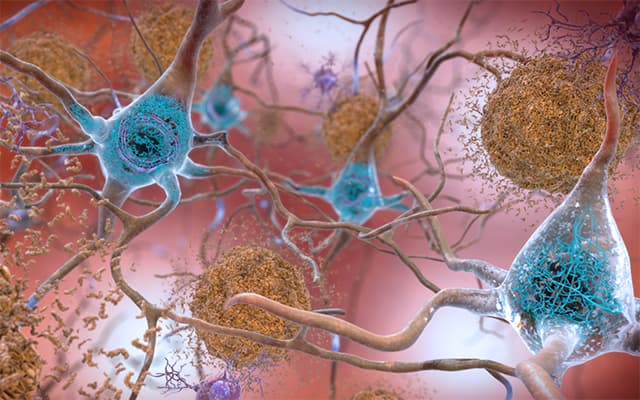
In this artist’s rendering, amyloid plaques are interspersed among neurons. These aggregates of misfolded proteins disrupt and kill brain cells, and are a hallmark of Alzheimer’s disease. Photo credit: National Institute of Aging
Amyloid plaques are pathological hallmarks of Alzheimer’s disease (AD) — clumps of misfolded proteins that accumulate in the brain, disrupting and killing neurons and resulting in the progressive cognitive impairment that is characteristic of the widespread neurological disorder.
In a new study, published March 2, 2021 in the Journal of Experimental Medicine (JEM), researchers at University of California San Diego School of Medicine, Massachusetts General Hospital and elsewhere have identified a new drug that could prevent AD by modulating, rather than inhibiting, a key enzyme involved in forming amyloid plaques.
In studies using rodents and monkeys, the researchers report the drug was found to be safe and effective, paving the way for possible clinical trials in humans.
“Alzheimer’s disease is an extraordinarily complex and multi-faceted condition that has, so far, defied effective treatment, let alone prevention,” said senior author Steven L. Wagner, PhD, professor in the Department of Neurosciences at UC San Diego School of Medicine. “Our findings suggest a potential therapy that might prevent one of the key elements of AD.”
Amyloid plaques are composed of small protein fragments called amyloid beta (Aβ) peptides. These peptides are generated by enzymes called β-secretase and γ-secretase, which sequentially cleave a protein called amyloid precursor protein on the surfaces of neurons to release Aβ fragments of varying lengths. Some of these fragments, such as Aβ42, are particularly prone to forming plaques, and their production is elevated in patients with mutations predisposing them to early-onset AD.
Several attempts have been made to treat or prevent AD using drugs that inhibit either β-secretase or γ-secretase, but many of these drugs have proved to be highly toxic or unsafe in humans, likely because β-secretase and γ-secretase are required to cleave additional proteins in the brain and other organs.
Instead, Wagner and colleagues investigated the therapeutic potential of drugs known as γ-secretase modulators or GSMs, which instead of inhibiting the γ-secretase enzyme, slightly alter its activity so that it produces fewer Aβ peptides that are prone to form plaques while continuing to duties cleaving other protein targets.
“GSMs offer the ability to mitigate mechanism-based toxicities associated with γ-secretase inhibitors,” said Wagner.
In the new JEM study, researchers created a novel GSM and tested it on mice, rats and macaques. They found that repeated, low doses of the GSM eliminated Aβ42 production in mice and rats, without causing any toxic side effects. The drug was also safe and effective in macaques, reducing Aβ42 levels by up to 70 percent.
The novel GSM was then tested in a mouse model of early-onset AD, treating the animals either before or shortly after they began to form amyloid plaques. In both cases, the novel GSM decreased plaque formation and reduced plaque-associated inflammation, which is thought to contribute to the development of disease.
The findings suggest that the novel GSM could be used prophylactically to prevent AD, write the authors, either in patients with genetic mutations that increase susceptibility to AD or in cases where amyloid plaques have been detected by brain scans.
“In this study, we have pharmacologically characterized a potent GSM that, based on its preclinical attributes, appears to equal or exceed the potency of any previously tested GSMs,” said co-author Rudolph Tanzi, PhD, professor neurology at Harvard Medical School and director of the Genetics and Aging Research Unit at Massachusetts General Hospital.
“Future clinical trials will determine whether this promising GSM is safe in humans and could be used to effectively treat or prevent Alzheimer’s disease.”
An estimated 5 million Americans are living with AD. The number of people with AD doubles every five years beyond age 65, according to the Centers for Disease Control, with the total number of Americans with the disease projected to nearly triple to 14 million by 2060. Currently, there is no known cure, only symptomatic therapies.
Co-authors include: Kevin D. Rynearson, Olga Prikhodko, Yuhuan Xie, Phuong Nguyen, Mariko Sawa, Ann Becker, Brian Spencer, Jazmin Florio, Michael Mante, Bahar Salehi, Carlos Arias, Douglas Galasko and William C. Mobley, all at UC San Diego; Robert A. Rissman and Brian P. Head, UC San Diego and Veterans Affairs San Diego Healthcare System; Moorthi Ponnusamy and Gopal Thinakaran, University of South Florida; Can Zhang, Massachusetts General Hospital; Brenda Hug, Veterans Affairs San Diego Healthcare System; Graham Johnson, NuPharmAdvise, New Hampshire; Jiunn H. Lin, Biopharm Consulting Partners, Pennsylvania; and Steven K. Duddy, Integrated Nonclinical Development Solutions.
Funding for this research came, in part, from the Cure Alzheimer’s Fund, the National Institute of Neurological Communicative Disorders and Stroke, the National Institute of Aging, the NIH/NINDS Blue Print (grants NS 074501, U01AG048986, RO1AG055523, RO1AG056061) and the DH Chen Foundation.
MEDIA CONTACT
Scott LaFee
ucsdnews.ucsd.edu


